SPECIALTIES
Periodontics
Periodontal disease is a progressive inflammatory disease of the gums and tissue (bone) that supports the tooth. Periodontal disease is the No. 1 cause of tooth loss after age 30, and it is believed that 80% of the population under 30 years can suffer from this disease with varying degrees of severity and it is usually painless.
Causes of Periodontal Disease
The main cause of periodontal disease is plaque, a sticky, colorless film that is constantly formed on teeth. However, factors such as those mentioned below can also affect the health of your gums.
Smoke
Cigarette smoking is linked with many serious diseases like cancer, lung disease, cardiovascular problems, as well as many other health problems. In addition, smokers are at increased risk for periodontal disease. In fact, recent studies have shown that cigarette smoking may be one of the most important risk factors in the development and progression of periodontal disease.
Genetics
Recent surveys show that 1 / 6 of the population may be genetically susceptible to gum disease. Despite good hygiene and oral care, these people may be six times more likely to present periodontal disease. Identifying these people through rigid professional control before they present symptoms of the disease, and subject them to a previous treatment can help them to keep their teeth for a lifetime.
Pregnancy and Puberty
Brushing your teeth, flossing, a healthy diet and regular exercise are important for maintaining good health. However, at certain stages of the life of a woman, that care must be redoubled. Stages such as puberty and menopause or menstrual periods and pregnancy, are periods of intense hormonal changes that can affect various tissues throughout the body, including the gums. They can become sensitive and even react aggressively to the fluctuation in hormones, which increase susceptibility to periodontal disease. In addition, recent studies suggest that pregnant women who have periodontal disease also have seven times more chance of having a premature labor and low birth weight babies.
Stress
Stress is linked with many serious diseases such as hypertension, cancer, and many other health problems. However it is important to know that stress is also one of the most important risk factors to the development and progression of periodontal disease. Research shows that stress makes it harder for the body to fight infections, including periodontal diseases..
Drug
Some medications such as oral contraceptives, antidepressants, anticonvulsants, and certain drugs for cardiovascular problems, can affect your oral health. So you should also tell your dentist about medicines that you use, in the interview about the drugs
Bruxism or parafunction
Waking up with the masticatory muscles sore or someone observing you grind your teeth at night is a sign of bruxism or parafunction. Clenching or grinding the teeth, even if unconscious, submits the tissues around the teeth to excessive force and may hasten the destruction of periodontal tissues in case of illness.
Diabetes
Diabetes is a disease that alters the sugar levels in the blood. Diabetes develops by a deficiency in insulin production (a hormone that is the key component in the process of consumption of sugar by the body in the blood) or a body’s inability to use this insulin properly. According to the American Diabetes Association, approximately 16 million Americans have diabetes, yet more than half haven’t been diagnosed for this disease. If you are diabetic, you have a higher risk of developing infections, including periodontal diseases. These infections can impair the ability to produce and / or utilize insulin, which can complicate diabetes control, but also can make the infection more severe than in no diabetic individuals.
Malnutrition and other Systemic Diseases
As you know, a diet low in important nutrients can compromise the immune system and make it harder for the body to fight infections. Since periodontal disease is an infectious disease, malnutrition and diseases that interfere with your immune system can affect your oral health and may worsen the condition of your gums.
Periodontal Treatments
Treatment depends on the type of periodontal disease present and the severity of it.
There are many forms and stages of periodontal disease, the most common are:
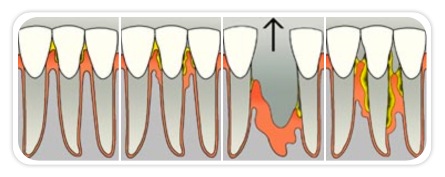
Gengivitis
The first stage of periodontal disease is a marginal inflammation of the gums caused by plaque. The gum will have a reddish color, will be inflamed and constantly will bleed when you brush and floss. This stage of the disease is reversible if treated before they evolved.

Mild periodontitis
Inflammation will spread to the supporting bone. Small bone loss and periodontal pockets may occur. It is also easily treated, but needs intervention under local anesthesia.
Moderate periodontitis
At this stage there is an increase regression of the gums, periodontal pockets of moderate to profound, bone loss from moderate to severe, purulent secretion, and tooth mobility. At this stage treatment is more interceptive, requiring few sessions under local anesthesia.
Severe periodontitis
This is the most advanced and serious stage of periodontitis. Deep pockets, increased tooth mobility, tooth extrusion and fistulae are present at this stage. Inflammation can develop bone loss, and if this inflammation continues it will have tooth loss. At this stage the treatment is aimed at keeping the elements that are still viable, extractions and implant are usually necessary. It is essential at this point the collaboration and changing habits of the patient.

For a correct diagnosis of periodontal disease professionals evaluate some items:
– Color, bleeding and gingival tissue condition
– Measurement of pockets
– Reviews of bone X-ray
– Dental mobility
– The amount of plaque present
– These items will determine the stage of the disease and proper treatment.
– Our staff will evaluate the periodontal status of our patients at each periodic visit, and through monitoring visits it becomes possible to assess whether progress is occurring or not.
PREVENTION
The best way to prevent periodontal disease and dental caries is the maintenance of good oral hygiene. Brush your teeth every day will remove a thin bacterial layer called dental plaque that settles on tooth surfaces. Use dental floss daily to remove plaque between teeth, these areas the toothbrush cannot reach.
Non-surgical treatments
Non-surgical treatments are the treatment of choice for patients who are in the early stages of the disease:
Oral Hygiene
prophylaxis
supra and sub gingival scraping
Oral Hygiene
If periodontal disease is in early stage (gingivitis), the professional will guide your oral hygiene and may prescribe oral rinse with mouthwash.
Prophylaxis
Prophylaxis consists of cleaning, fluoride application and polishing with a prophylaxis paste and rubber. This step is done in conjunction with scaling, so prevention is effective.
Supra Gingival Scalling
Consists of the meticulous removal of toxins, microorganisms and dental plaque. This procedure is done to remove biofilm, plaque and toxins, in order to obtain a response from the body recovering from bacterial invasion.
Subgingival
Consists of the meticulous removal of toxins, microorganisms not visible to the naked eye present in the gum attached to the tooth. Tartar present in this way promotes the formation of so-called periodontal pockets. These bags should be treated periodically with scraping sessions, varying the number of sessions according to the severity of each case.
Surgical treatments
– Curettage or sub-gingival scraping
– Gingivectomy
– Gingivoplasty
– Gingivoplasty in restoration procedure
– Gingivoplasty or plastic surgery of the gum
– Increase of crown
Curettage or sub-gingival scraping
Gingival curettage removes a thin layer of tissue present in periodontal pockets in order to completely eliminate bacteria and damaged tissue. It can be done with ultrasound or root planing with specific curettes. But it is necessary to address deeper in the gums, usually under local anesthesia or sedation with nitrous oxide.
Gengivectomy
Gingivectomy is a surgical procedure that remodels the gingival tissue with cosmetic, physiological and functional purposes. Some indications of gingivectomy are: endodontic treatment, severe periodontitis, excess of gum tissue and others.
Gengivoplasty or plastic surgery of the gum
It is usually done with local anesthesia or sedation with nitrous oxide, and is recommended for remodeling the irregular and aesthetically unsatisfactory gingival tissue. It is a simple surgical procedure that adjusts the position of the gum around the tooth in question. A functional gingivoplasty will help you regain your beautiful smile, eat and speak with comfort and confidence. The gingivoplasty is indicated in the preparation of the tooth restorations and cosmetic procedures on the gums.
Gengivoplasty in restoration procedure
When suffering from dental caries below the gum line, usually there is insufficient bone structure for restoration or prosthetic crown. So it is necessary to do a gingivoplasty of the gum. The end of the tooth is exposed so you can restore it correctly without damaging the periodontal health.
Gengivoplasty in cosmetic
Usually done to correct the known gummy smile that hides the tooth below the gum excess. The gummy smile is the excess of gum over the tooth, which causes it to be shorter. During the procedure the gums are removed, exposing the tooth that was covered, returning the smile and confidence. This can be done on a tooth or a teeth sequence to return the natural smile.

Increase crown
is a surgical procedure that remodels the bone tissue around the tooth for cosmetic, physiological and functional purposes. Some indications of increased crown: Exposure of the end of teeth for restorations and root canal treatment, increasing the space for making prosthetic implant, removal of periodontal pockets and others.
